Have you noticed your legs feeling more tired than usual? Do simple tasks like climbing stairs, getting out of a chair, or walking to the mailbox feel harder than they used to? You’re not alone. Many adults over 60 experience gradual leg weakness—but in most cases, it’s not just “old age.”

Subtle changes in movement, nutrition, and nerve health can quietly chip away at strength and balance. The good news? Once you know the causes, you can take simple, effective steps to keep your legs strong and your mobility steady.
Let’s explore six surprising reasons your legs might be weakening—and what you can do, starting today, to move with more confidence.
1. Not Enough Muscle-Activating Movement

Daily walks are great for heart health, but they don’t always target the deep stabilizing muscles that keep your legs strong. Without regular strength training, muscle mass naturally decreases with age—a process called sarcopenia—making legs feel weaker over time.
What to do:
- Add 10–15 minutes of gentle, leg-focused strength work 3–4 times a week.
- Try sit-to-stand reps from a sturdy chair, calf raises at the counter, or seated leg extensions.
- Use light ankle weights or resistance bands for added challenge.
Why it matters:
Research in the Journal of Aging and Physical Activity shows that consistent resistance training can significantly slow age-related muscle loss.
2. Poor Circulation in the Lower Body
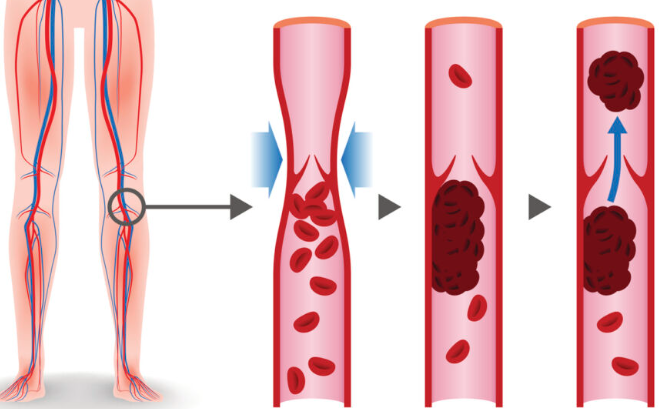
Reduced blood flow can make legs feel heavy, tired, or crampy even after short periods of activity. This may be linked to peripheral artery disease (PAD) or simply sitting too long without movement.
Warning signs:
- Cold feet or toes
- Calf cramps when walking
- Swelling around the ankles
What to do:
- Elevate your legs while resting.
- Take walking or stretching breaks every hour.
- Do ankle pumps or circles while sitting.
- Avoid crossing your legs for extended periods.
If symptoms persist, ask your healthcare provider about a circulation check.
3. Low Vitamin D and Calcium Levels

Strong bones and well-functioning muscles rely on vitamin D and calcium—two nutrients that become harder to maintain with age. Low levels can lead to bone thinning, weakness, and a higher risk of falls.
How to boost levels:
- Spend 15–20 minutes in sunlight daily (when possible).
- Eat calcium-rich foods like leafy greens, dairy, or fortified plant milks.
- Ask your doctor to check your vitamin D levels and recommend supplements if needed.
According to Harvard Health Publishing, vitamin D also plays a key role in regulating muscle contractions and balance.
4. Weak Nerve-to-Muscle Communication
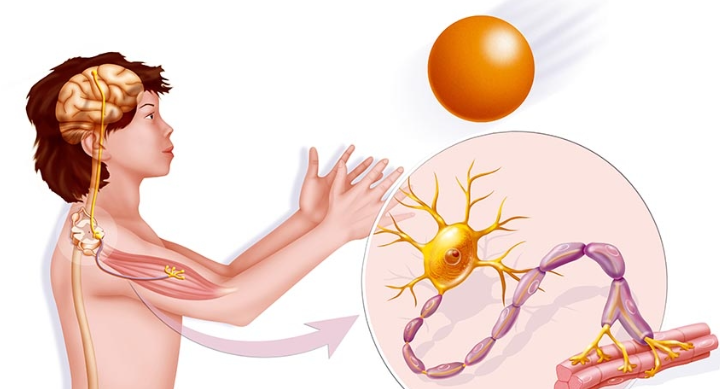
When nerves can’t send strong signals to muscles, movements may feel slower or less coordinated. This can happen due to diabetes, vitamin B12 deficiency, or certain medications.
What to do:
- Manage blood sugar if you have diabetes or prediabetes.
- Eat foods rich in B12 like fish, eggs, and fortified cereals.
- Ask your doctor for a B12 test if you follow a vegetarian or low-meat diet.
If you experience numbness, tingling, or burning sensations, consult your healthcare provider.
5. Neglecting Balance Muscles

Leg strength alone isn’t enough—smaller stabilizing muscles around the hips and core help prevent falls and keep movements coordinated. Ignoring them can lead to wobbliness and instability.
Signs of neglected balance muscles:
- Feeling unsteady when turning quickly
- Needing to hold onto furniture when standing
- Wobbling during basic stretches
Exercises to try:
- Stand on one foot while holding a countertop (10–30 seconds each side)
- Side leg lifts
- Gentle yoga or tai chi
The National Institute on Aging recommends balance training as a core part of senior fitness.
6. Not Enough High-Quality Protein

Muscles need protein to repair and rebuild. If your meals are low in protein—or if your body isn’t absorbing it efficiently—you may experience gradual strength loss.
How to get more:
- Include protein at every meal.
- Mix animal and plant-based sources: eggs, fish, poultry, legumes, tofu, dairy.
- Add Greek yogurt, cottage cheese, or a protein smoothie to breakfast.
Note: If you have kidney issues, talk to your doctor before increasing protein intake.
Your Step-by-Step Action Plan
- Identify one reason from this list that matches your situation.
- Set a small, specific goal—like doing 10 chair sit-to-stands each morning.
- Track your progress weekly and celebrate improvements.
You can rebuild strength, stability, and confidence at any age. The key is starting with small, consistent changes and giving your body the support it needs to stay active.
Every strong step you take today is an investment in your independence tomorrow.